The government’s age-centred vaccine rollout pushed the more youthful Māori population to the back of the vaccination queue, which means most Māori will be last in line for boosters as Omicron arrives in this country.
Britain allows boosters after three months for vulnerable groups. The government must immediately adjust to this setting for the Māori rollout.
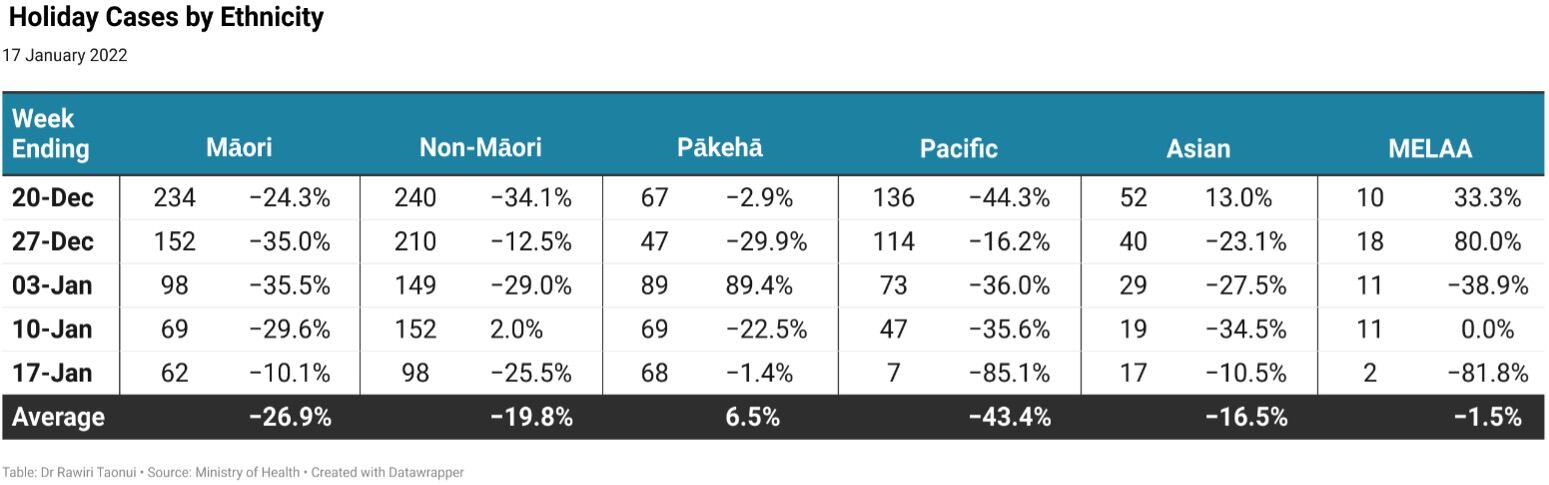
In the week ending Monday, January 17 there were 62 new Māori community cases and 98 non-Māori cases. With 68 community cases, Pākehā topped the highest number of weekly cases for the first time since the outbreak began in August.
Over the past five weeks since the opening of the Auckland border, Māori cases have declined by an average of 26.9% per week compared to 19.8% per week for non-Māori. Pacific cases were the only cases with a higher decline than Māori.
Pākehā cases increased by 6.5% over the same period because of an 89.4% spike between Boxing Day and the New Year.
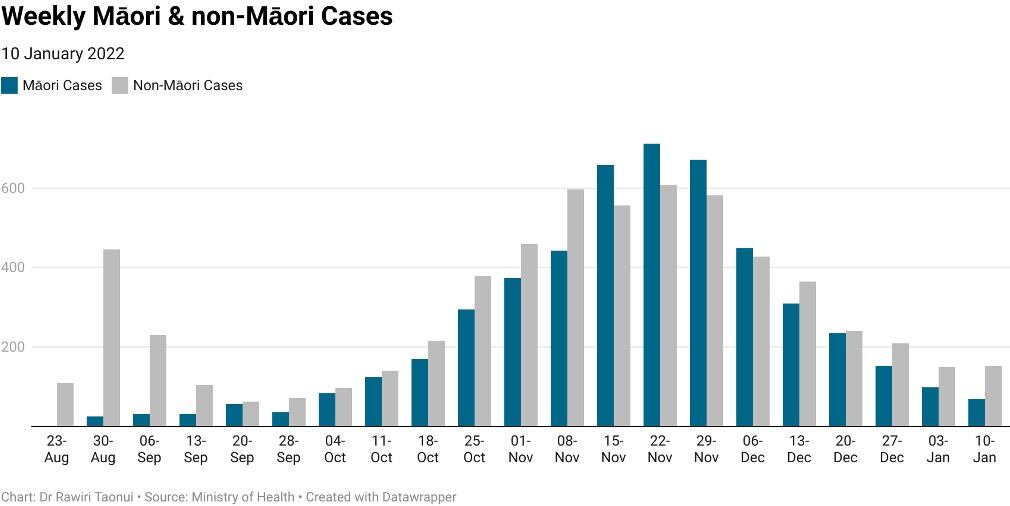
The following chart compares Māori and non-Māori/Pacific cases over the 22 weeks of the current outbreak. This confirms that, after Māori dominated the middle part of the outbreak, cases have fallen faster than that for all other ethnicities combined.
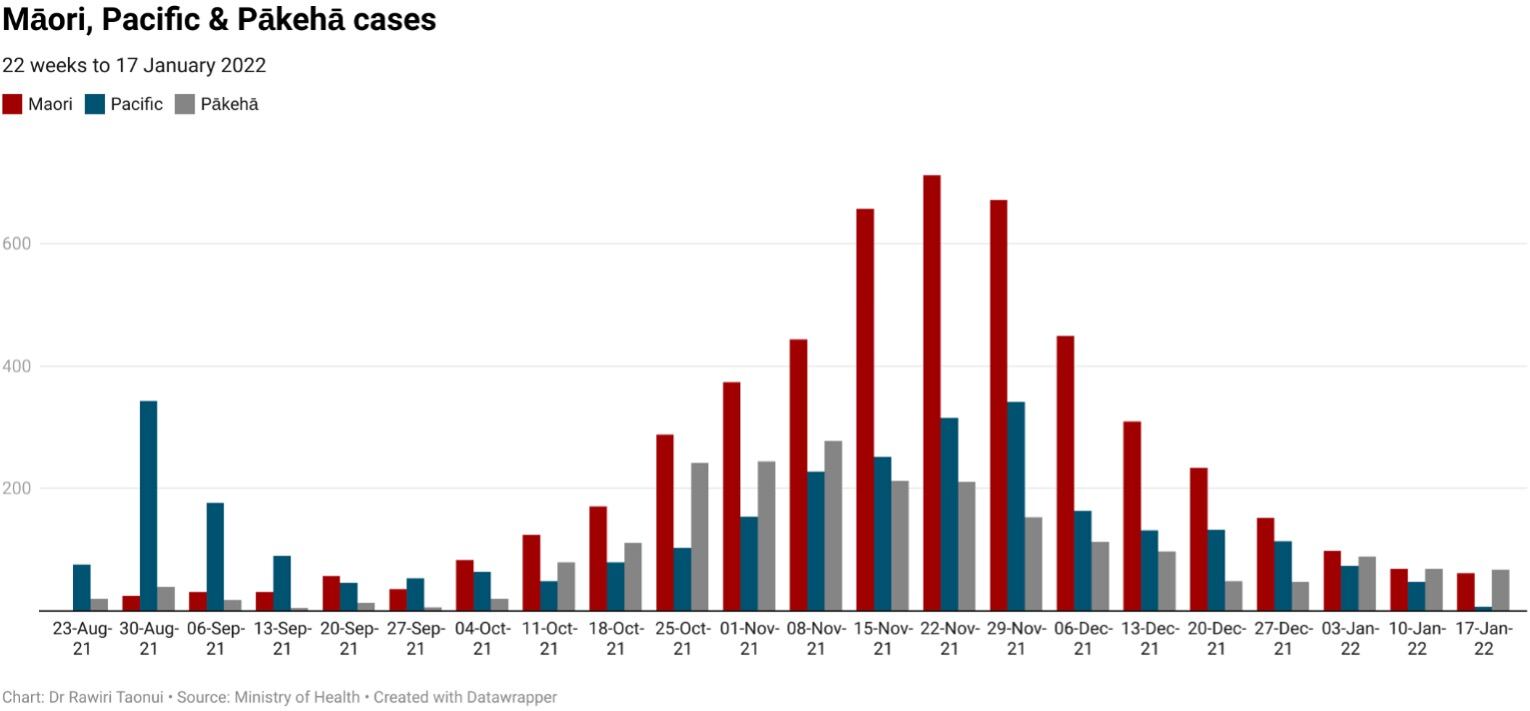
The next chart compares Māori, Pacific and Pākehā weekly cases during this outbreak.
Pacific cases dominated during August and early September. Māori cases dominated numbers for 15 consecutive weeks after the government took Auckland to Alert Level 3 in September.
From late November cases declined among all ethnicities with the largest decrease occurring in the lower-vaccinated but more vigilant Māori and Pacific communities.
Māori cases
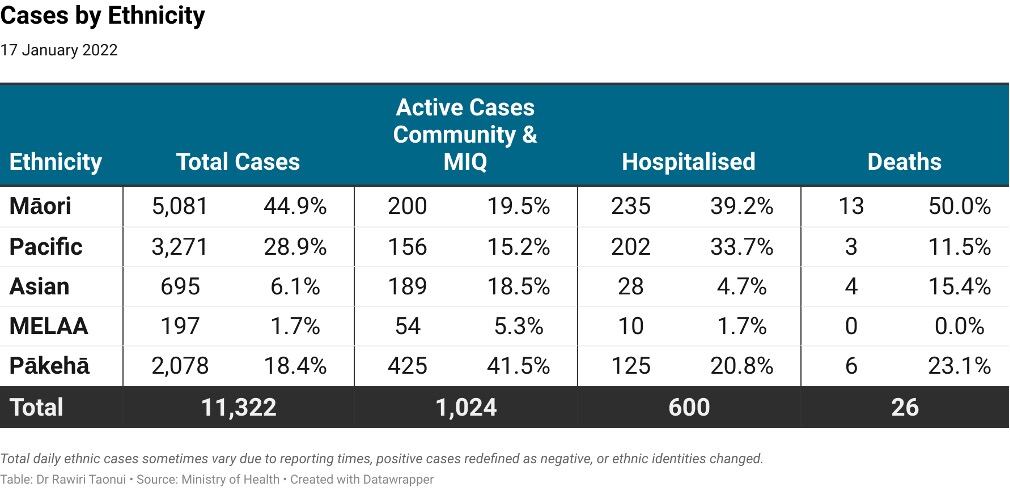
As of Monday, Māori were 44.9% of all cases, 19.5% of active cases, 39.2% of hospitalised cases and 50% of deaths.
Since December 21 Māori active cases have fallen 72.9% from 708 to 200 because of higher holiday vigilance while Pākehā active cases have risen 71.2% from 247 to 425 because of higher Pākehā cases in holiday spots and higher numbers of Pākehā among New Zealanders returning from overseas.
Covid risk
Measured by 100,000 of population, Māori are 10.4 times more likely to become infected, 8.0 times more likely to be hospitalised and 9.2 more likely to die.
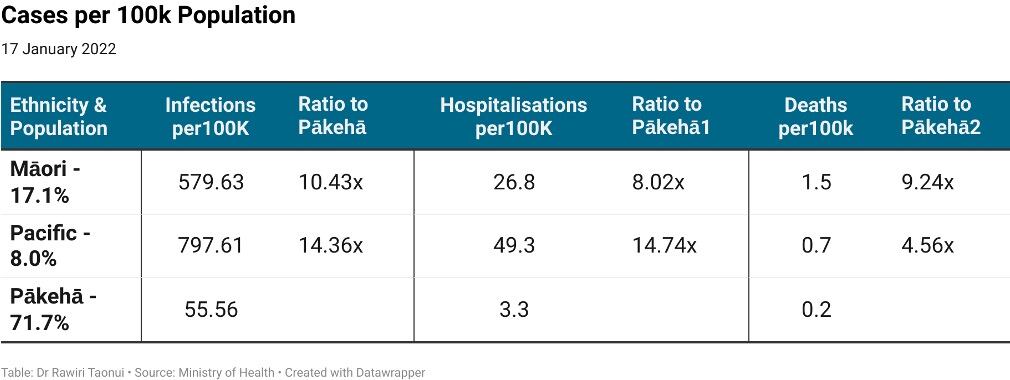
Pacific peoples, the next most Covid-19 impacted cultural group after Māori, have higher infections and hospitalisations because of the exceedingly low vaccination rates at the beginning of the outbreak in the early August outbreak.
Vaccination status
The first three columns in the following table compare Covid-19 cases by vaccination status between Māori, Pacific peoples, and non-Māori/Pacific. The standout feature is that fully vaccinated Māori (10.9 per cent) have an infection rate of one-third that of non-Māori/Pacific (30.4 per cent).
The two columns on the right show that the non-fully vaccinated Māori (unvaccinated, under-12 years and partially vaccinated) contribute a disproportionately high percentage of cases to the national total.
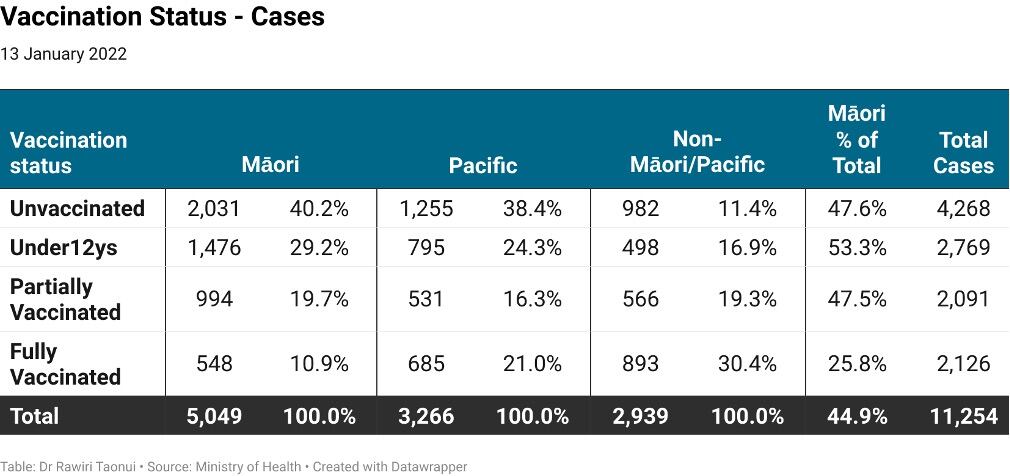
The next table compares the vaccination status of those who were hospitalised. Fully vaccinated Pacific peoples (5.4 per cent) and Māori (5.6 per cent) are less than half the hospitalisations of fully vaccinated cases in the non-Māori/Pacific communities (13.0 per cent).

Nevertheless, fully-vaccinated Māori (28.9 per cent) form a considerable proportion of hospitalisations again showing our overall Covid-19 vulnerability.
Māori vaccination
The Ministry of Health uses the Health Services User index (HSU) to calculate vaccination numbers. The HSU is based on the number of people who used the health system in 2020. This excludes those who did not use health services because they were extremely healthy, did not trust the system or were too poor. This creates an undercount. We see an undercount in other ethnicities, for example, the Ministry HSU calculates the Asian population at 598,00 but providers have vaccinated more than 630,000.
Comparing the HSU with the 2021 NZ Statistics Estimate of the Resident Population (ERP), there is a maximum potential Māori undercount of 102,700 including 12,420 young people in the 5 to 11 years age group. This undercount is concentrated in upper-North Island DHBs, Māori population regions, high Māori youth populations, areas of significant deprivation, and among Māori men.
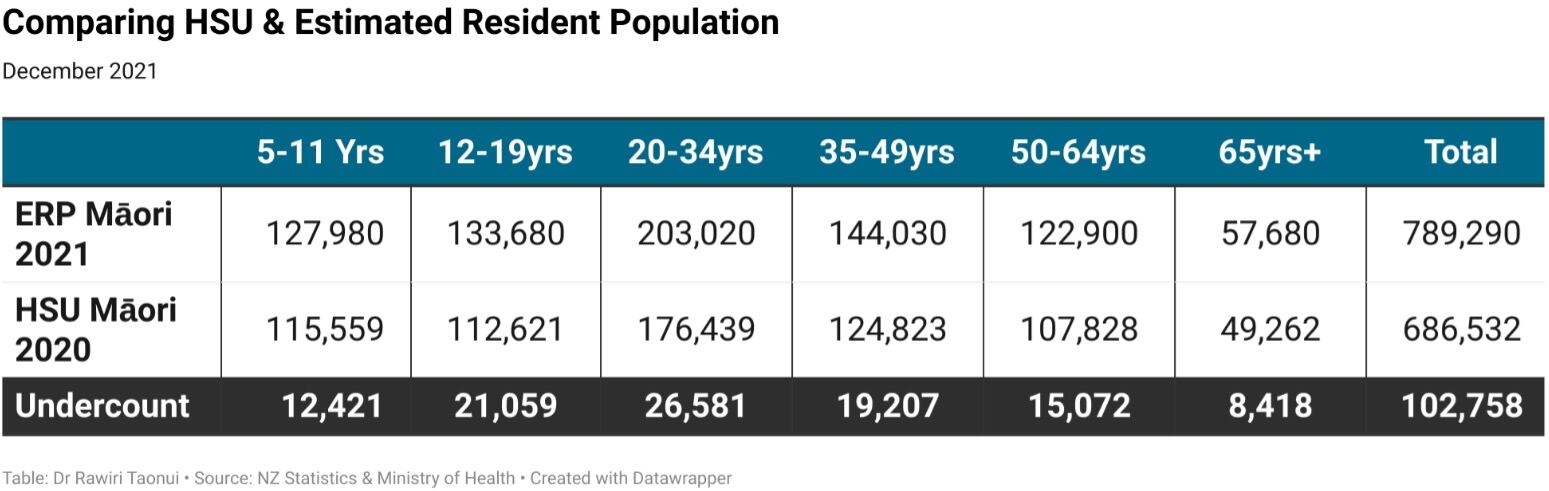
The ministry has not yet included the 5-to-11-years age group in daily reported vaccination numbers. Until then, I am using a conservative minimum accurate estimate of the undercount of 46,000.
On that basis, 82% of Māori have received at least one dose of the Pfizer vaccination and 77% are fully vaccinated (below).
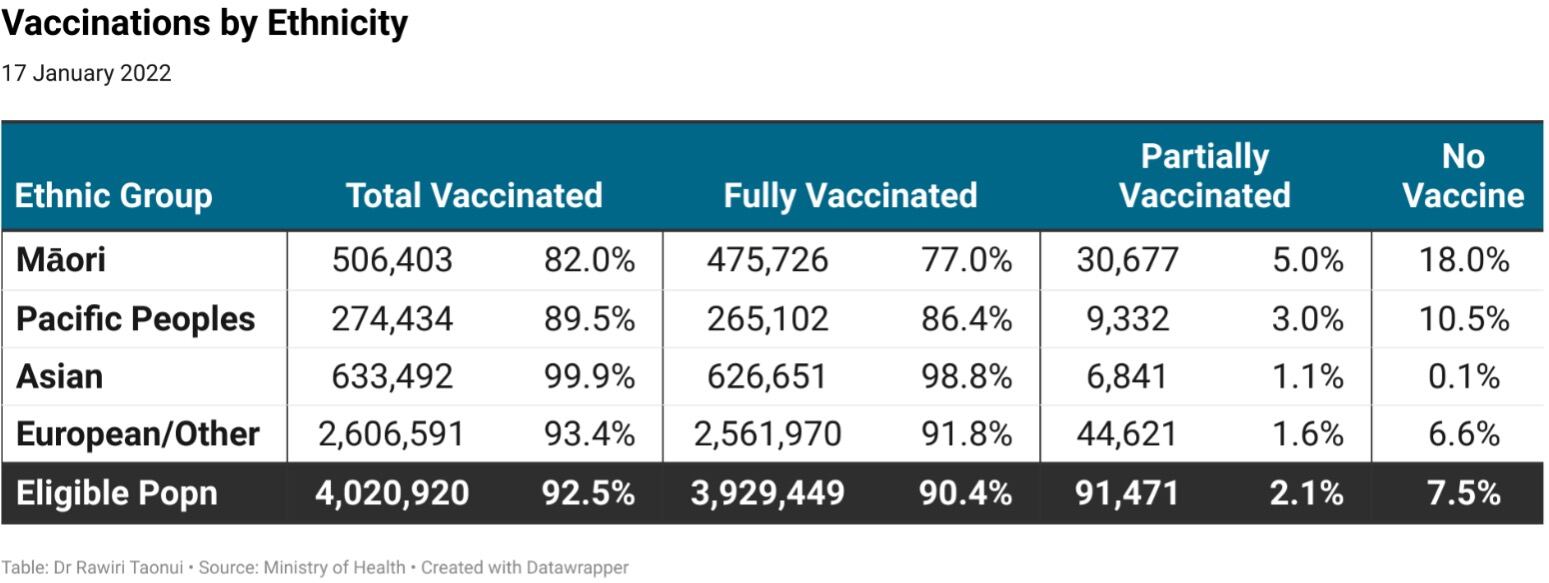
Respectively, this places Māori just over 10% behind the national rate for at least one dose, and 14.8% behind on double vaccination.
Despite those numbers, Māori health providers are making a credible effort to close the gap in vaccinating more than 100,000 Māori since November 1. The percentage increase of 26.6% is four times higher than the increase in Pākehā vaccination and higher than that for all other ethnicities combined.
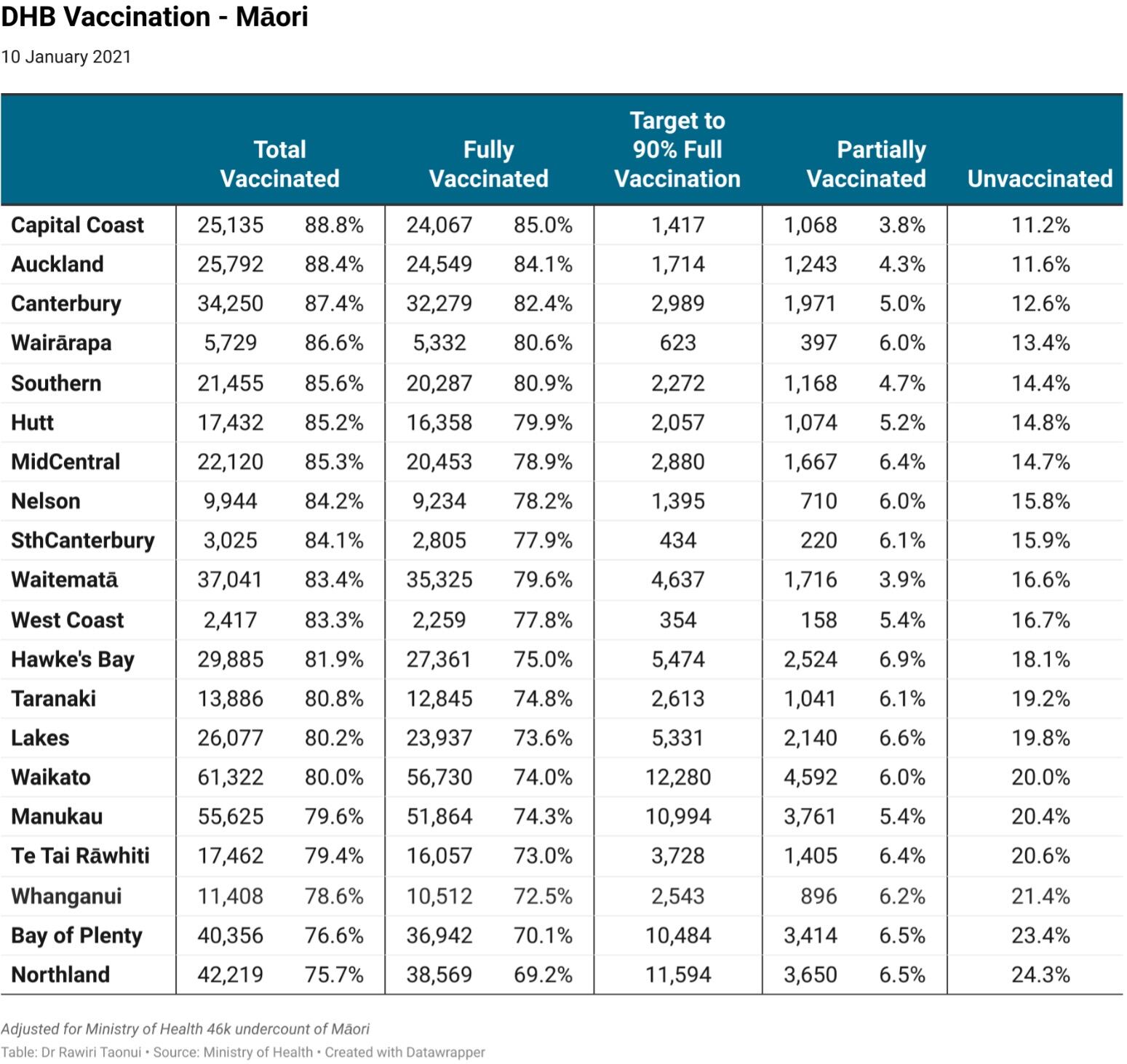
By DHB
Māori have passed 80% by at least one vaccination in 16 DHBs with only Te Tai Rāwhiti, Whanganui, the Bay of Plenty and Northland below this mark. Capital Coast, Auckland, Canterbury and the Wairārapa are closing on 90%.
Eight DHBs have passed 80%double vaccinated with Capital & Coast the closest to 90%. The Whanganui, Bay of Plenty and Northland have moved above 70%, which is promising but still well behind the national average.
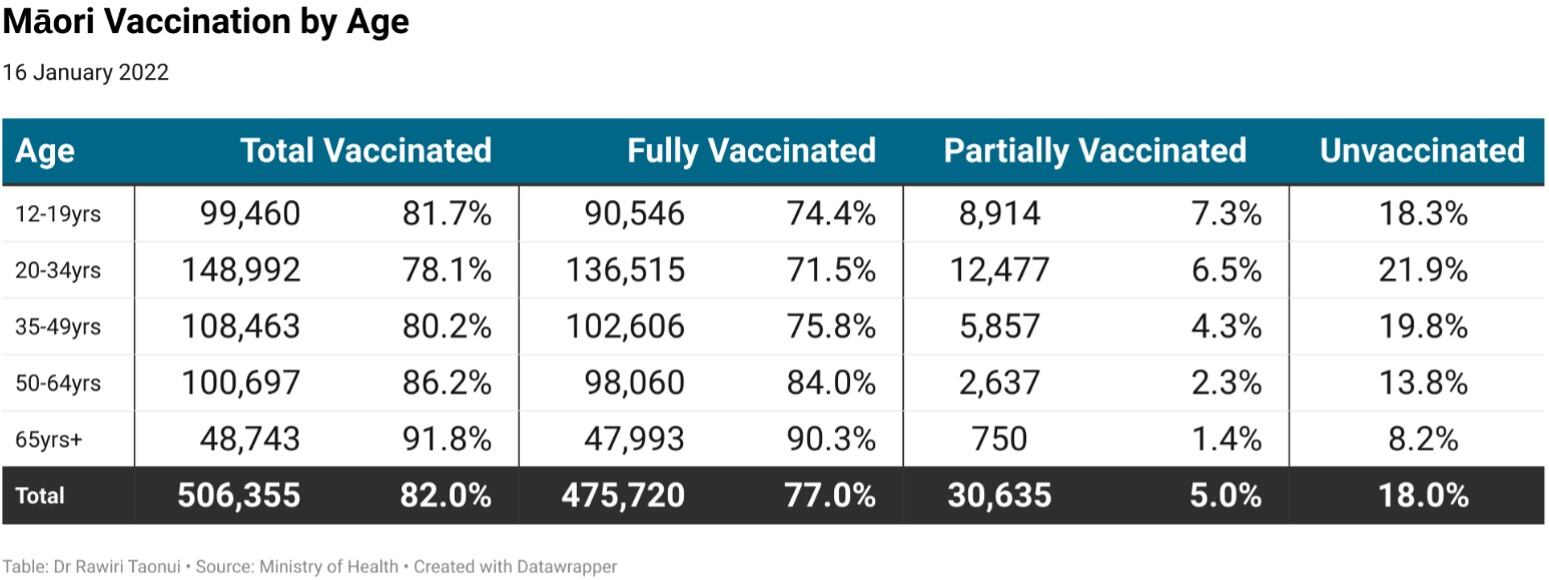
By age
Over 65-year-old Māori have reached 91.8% total vaccination and 90.3% full vaccination. Youngatira youth-led vaccination campaigns like IraDot have made a huge contribution to vaccinating Māori aged between 12 and 34 years of age who comprise over 70,000 of the 100,000 Māori vaccinated since November 1.
Booster and tamariki vaccination
The booster vaccination rollout is well underway. Although beyond the Monday, January 17 alignment of this report, there are early signs of continuing inequality in the rollout.
Preliminary data from the Auckland 5 to 11 years-old rollout shows tamariki Māori numbers at 50% of those for non-Māori/Pacific children. This is a real concern. The government and ministry must appoint a tamariki Vaccination Monitoring Group with both access to data and officials and the government and do so now.
Unconfirmed preliminary national data shows a 35% booster uptake for eligible Asian, 57% for Pākehā, 44% for Māori and 34% for Pacific. The very urgent concern is that the age-centred vaccine rollout pushed the more youthful Māori population to the back of the vaccination queue meaning most Māori will be last in line for boosters.
Further, the 100,000 Māori vaccinated after November 1, constituting 20% of all vaccinated Māori, will not become eligible for their booster shots until March 1. Given regular breaches of Omicron into the community, this will be too late to avert a disaster.
Britain allows boosters after three months for vulnerable groups. The government must immediately adjust to this setting for the Māori rollout.
Aotearoa
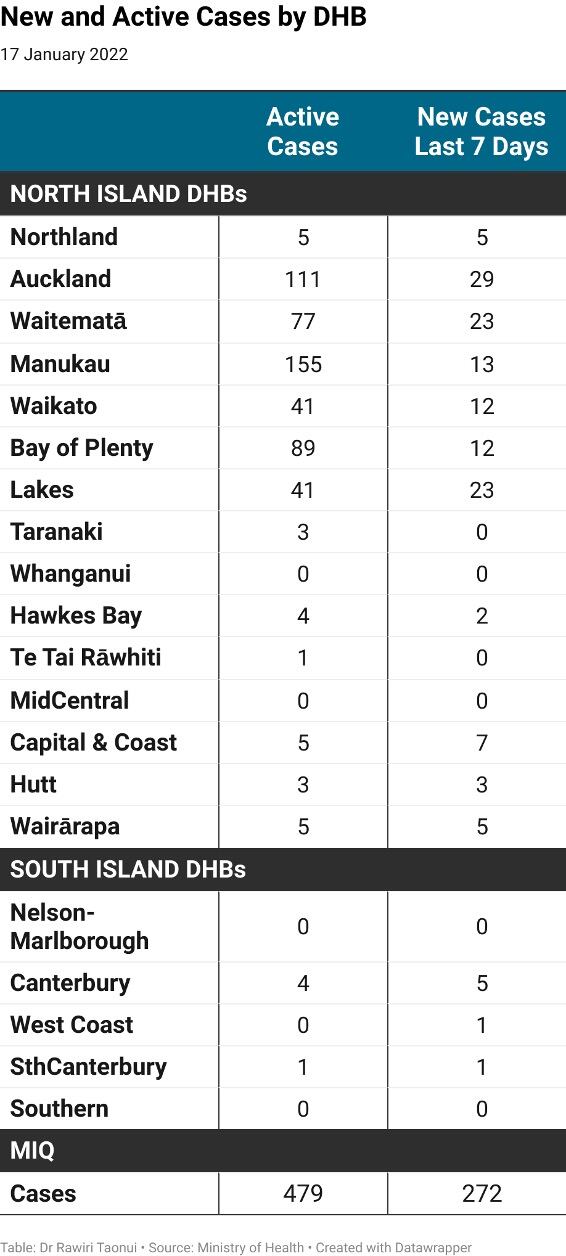
While cases were lower last week, they were geographically more widespread across 16 of 20 District Health Boards (DHBs). The highest new and active cases centre on the six DHBs between Auckland and the Lakes.
The overall number of cases is lower than in November meaning that the national vaccination programme, which is higher than the 66 per cent average in upper-income countries, has been effective. However, the wide geographic distribution of cases also means the Traffic Light System is facilitating the movement of the virus around the country.
Coupled with continuing breaches of cases from Managed Isolation and Quarantine, Omicron has the potential to ignite a significant outbreak across the country within an abbreviated period.
Noho haumaru, stay safe.
Dr Rawiri Taonui