Unvaccinated Māori are most at risk of catching Omicron, which will hit large numbers of Māori self-isolating at home. Phase 3 leaves lower-resourced, less financially secure Māori to self-manage testing, illness, and household contacts.
Protect whakapapa and whānau. Protect tamariki. Prioritise booster and tamariki vaccinations. Support and care for the unvaccinated, if necessary, respect the right of unvaccinated adults to live with the consequences of their decision.
Māori have put up a formidable Covid-19 response. There is strength in our communities and abundant leadership young and old.
This is our 1918 revisited.
Aotearoa has moved to Phase 3 of the Omicron Response. This means:
- Only confirmed cases and their household contacts are required to isolate. Isolation is for 10 days.
- All other contacts are to monitor symptoms but do not have to isolate.
- Rapid Antigen Tests (RATs) will become the primary form of testing in the community.
- RATs will be available from thousands of sites around the country including GP practices, pharmacies, and workplaces.
- Retail outlets will sell approved RATs from March.
- Those who test positive will self-report and self-notify their close contacts.
- Ministry of Health PCR testing and contact tracing resources will now focus on high-risk locations such as hospitals and aged care facilities.
- Advice on self-isolation is available here.
- A basic self-isolation plan is available here.
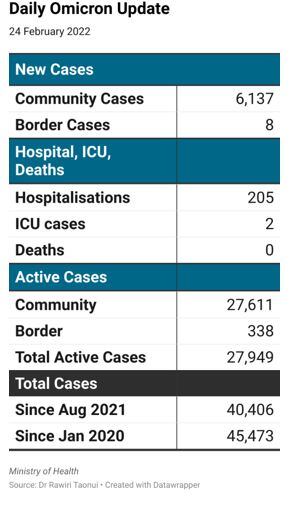
There were 6,137 new community cases yesterday. There are 205 people in hospitals and two in ICU. There are 27,611 active cases in the community.
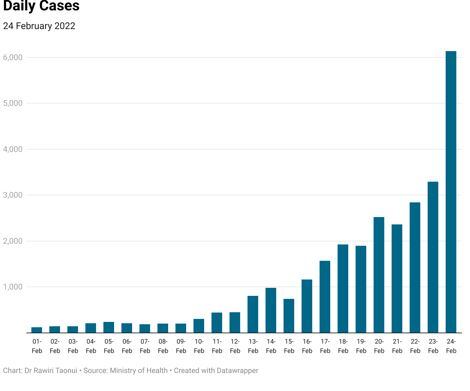
Omicron took 15 days to go from 126 cases on February 1 to pass 1,000 daily cases on February 16, five days to pass 2,000, three days to reach 3,000, and one day to double to 6,000 cases.
Modelling from Te Pūnaha Matatini predicts the Omicron outbreak will peak at 10,000 to 30,000 cases a day in mid-March.
Cases are running ahead of the lower 10,000 cases per day estimate. We will pass this mark within the next week.
Ethnic trends
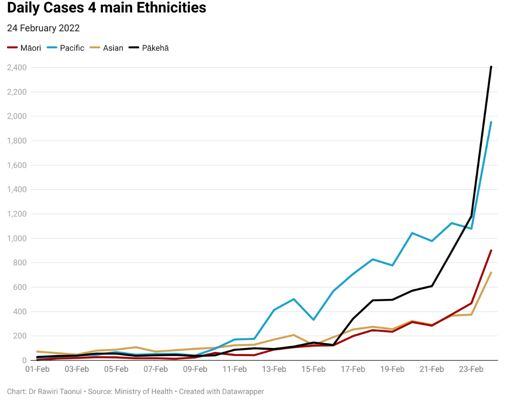
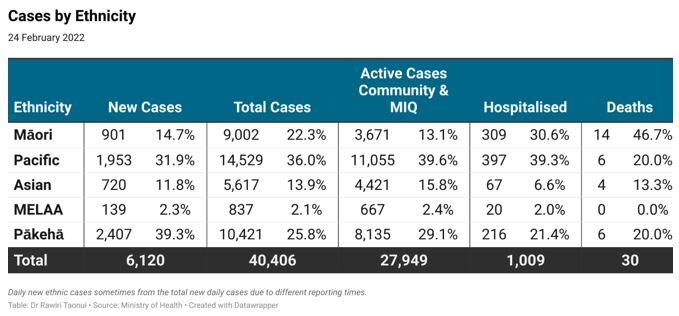
Pacific peoples dominated daily cases during the middle of this month.
Over the past two days, cases in the Pākehā community have set consecutive records with 1,182 and 2,407 new cases.
Māori have had the lowest cases of the four main ethnicities for most of this month.
This reflects the success of the early December $120 million Delta funding for Māori, and the work of Māori health providers, leaders, and communities in achieving the fastest decline in cases of all ethnicities during December.
There were 901 new cases in the Māori community yesterday. Māori cases have now passed those in the Asian community.
With lower overall vaccination rates, vaccination resistance in some DHBs and vulnerabilities in health and housing, Māori cases will rise more steeply, particularly when transfer occurs into provincial, urban-rural, and remote areas.
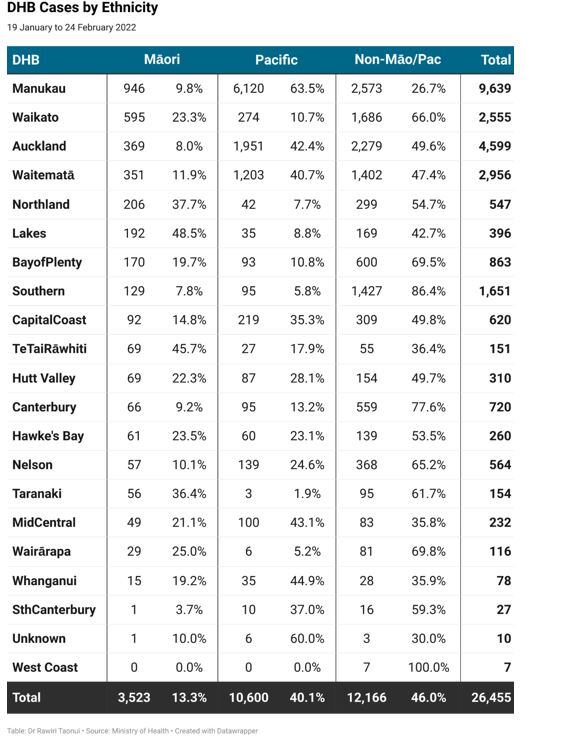
Current cases
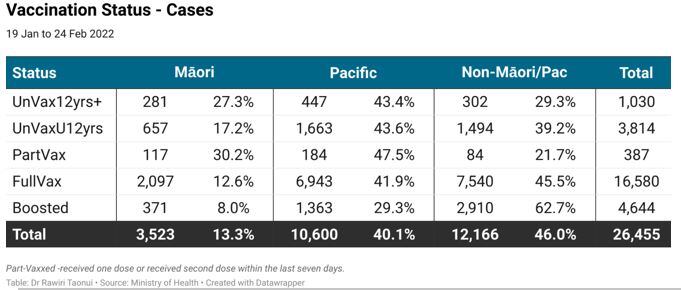
The following table shows new cases by vaccination status and ethnicity since January 19.
Overall, there are many more cases among the vaccinated community because the vaccinated are now 80.5% of the total New Zealand population.
The strength of the December/January Māori Covid-19 response means Māori are just 13.3% of all new cases. This is lower than our 17.1% demographic and 3.5 times lower than non-Māori/Pacific.
Unvaccinated 12yrs+ Māori (27.3%) and partially vaccinated Māori (30.2%) respectively contribute 1.6 times and 1.8 times our demographic to the national total.
Fully vaccinated (12.6%) and boosted Māori (8.0%) contribute much lower than our demographic and respectively are 3.6 times and 7.8 times lower than non-Māori/Pacific (45.5% and 62.7%).
Hospitalisations
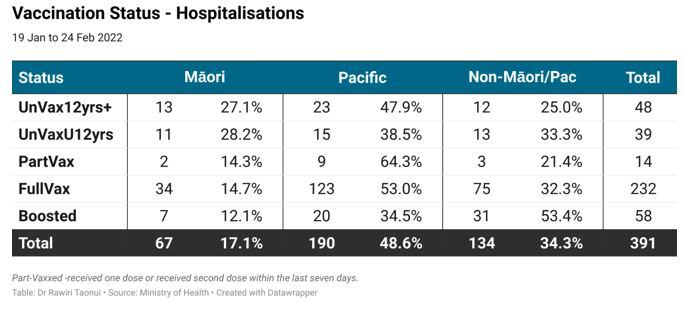
The following table shows new hospitalisations by vaccination status and ethnicity since January 19. The numbers show unvaccinated Māori have a higher risk of hospitalisation.
Despite lower Māori cases this month, unvaccinated Māori 12yrs+ (27.1%) saw more hospitalisations than the entire non-Māori/Pacific community (25.0%).
Unvaccinated tamariki Māori (28.2%) have similar hospitalisations to non-Māori/Pacific (33.3%).
By contrast, Māori hospitalisations for fully vaccinated (14.7%) and boosted (12.1%) are respectively 2.2 and 4.4 times lower than for non-Māori/Pacific (32.3% and 53.4%).
Since August 2020
Pacific peoples are the most impacted group in the current outbreak with 14,529 total cases.
Māori have the third-highest number of cases behind Pākehā.
Māori have the lowest number of active cases because of the excellent mahi in our communities during December/January.
Māori remain the second-highest number of hospitalised cases because of the extremely high cases in our community between September and November last year.
Update on deaths
The Ministry of Health has updated the age and ethnicity of deaths that occurred in January.
There have been 56 deaths since Covid-19 first arrived in Aotearoa. Māori are 33.9% of all deaths (19).
Some 30 of those deaths have been during the Delta–Omicron outbreak which began on August 17 last year. Māori accounted for 14 (46.7%) of those deaths.
Of the 11 Delta-Omicron deaths after December 8, eight were Māori.
Deaths during Omicron will be higher for Māori.
Current risk
On current case numbers and outcomes per 100,000 of population, Māori are 3.7 times more likely than Pākehā to be infected with Covid-19, 6.1 times more likely to be hospitalised and 10.0 times more likely to die.
One in 22 of every Māori who has been hospitalised during this outbreak has died compared to one in every 36 Pākehā.
Māori make up the largest proportion of younger deaths.
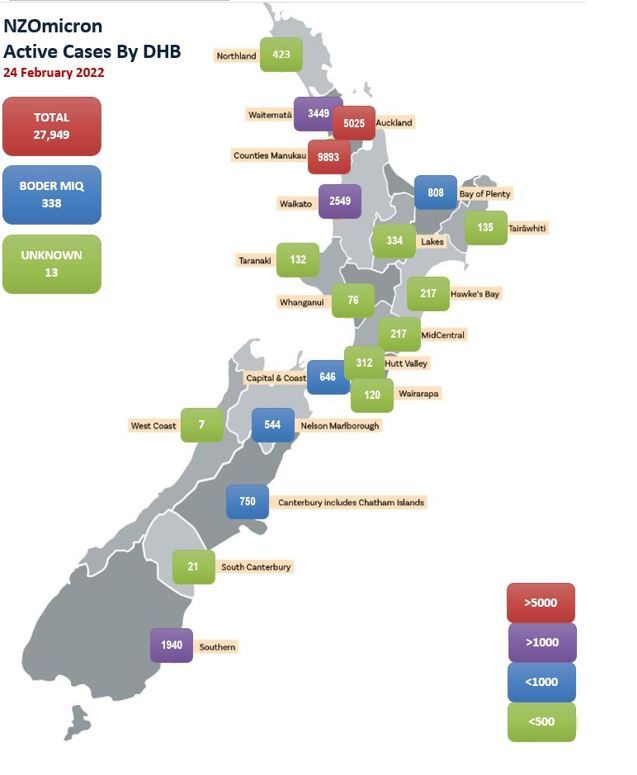
Active cases
Some 20,900 active community cases are in the Auckland and Waikato District Health Boards (DHBs).
Numbers are lower in the regions because of lower populations and distance from larger urban centres. Numbers will grow significantly over the next week.
Māori cases by DHB
The following table shows the number and percentage of Māori cases in each DHB compared to Pacific peoples and non-Māori/Pacific.
The pattern is higher Māori cases in high population areas (as expected) but also higher Māori cases in under-vaccinated Māori DHBs like Northland, Lakes, and the Bay of Plenty.
The unvaccinated are at most at risk of illness and hospitalisation.
This is our 1918
Māori face the greatest test with Omicron. Omicron is hyper-transmissible because of its enhanced ability to evade natural and vaccine-stimulated antibodies.
Most cases will be mild. The sheer number of cases will, nevertheless, mean many more will require hospital treatment than we have seen before. There will be more deaths, not on the 1918 Spanish Flu scale, but more than so far with Covid-19.
Māori have put up a formidable Covid-19 response. Whānau Ora, Te Whakakaupapa Urutā, the Iwi Leaders Pandemic Response Group, the Māori Council, the National Māori Authority, Māori paediatricians, Māori pharmacists, a host of others have been totally awesome. There is strength in our communities and abundant leadership young and old.
Unvaccinated Māori are most at risk. Omicron will hit large numbers of Māori self-isolating at home. Phase 3 leaves lower-resourced, less financially secure Māori to self-manage testing, illness, and household contacts.
Plan and prepare. Trust Māori providers. Work together. Make simple decisions based on what is best for your whānau and loved ones. Be willing to bend but not break the rules.
Protect whakapapa and whānau. Protect tamariki. Prioritise booster and tamariki vaccinations. Support and care for the unvaccinated, if necessary, respect the right of unvaccinated adults to live with the consequences of their decision.
Remember the costs of the last time hundreds of Māori self-isolated from disease. This is our 1918 revisited. Survive.
Noho haumaru, stay safe.
Dr Rawiri Taonui.