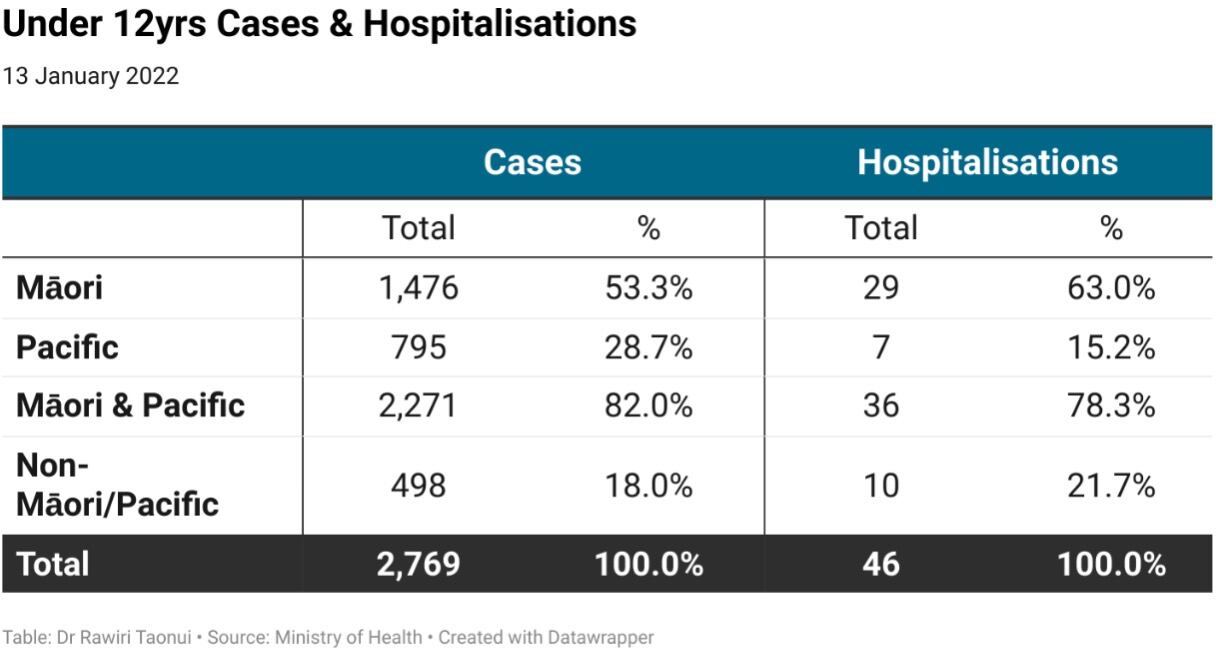
The government must accord tamariki Māori vaccination an urgent priority as New Zealand enters the five to 11 year-olds child rollout with our tamariki comprising 53.3 per cent of all cases and 63.0 per cent of all hospitalisations in the under-12 age group.
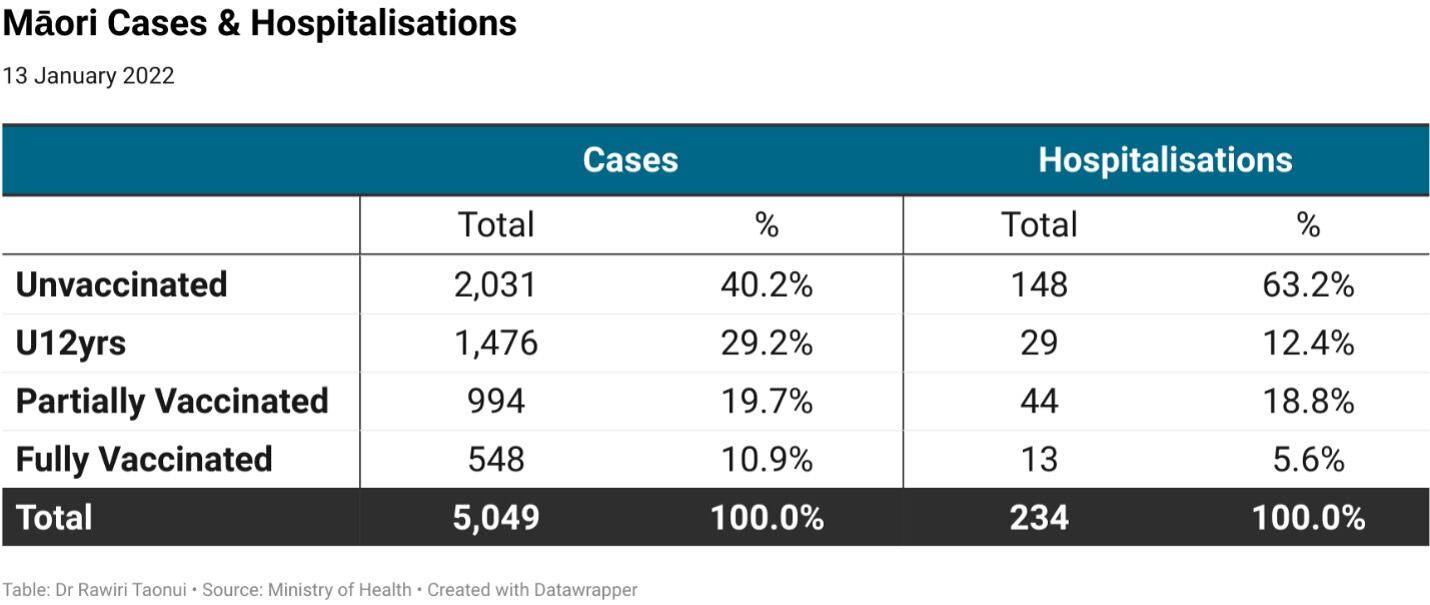
Tamariki are the taonga for the future of our whakapapa. At 24.6% of our population, Māori communities will be concerned that our tamariki are 29.2 per cent of all Māori cases.
Disproportionate burden
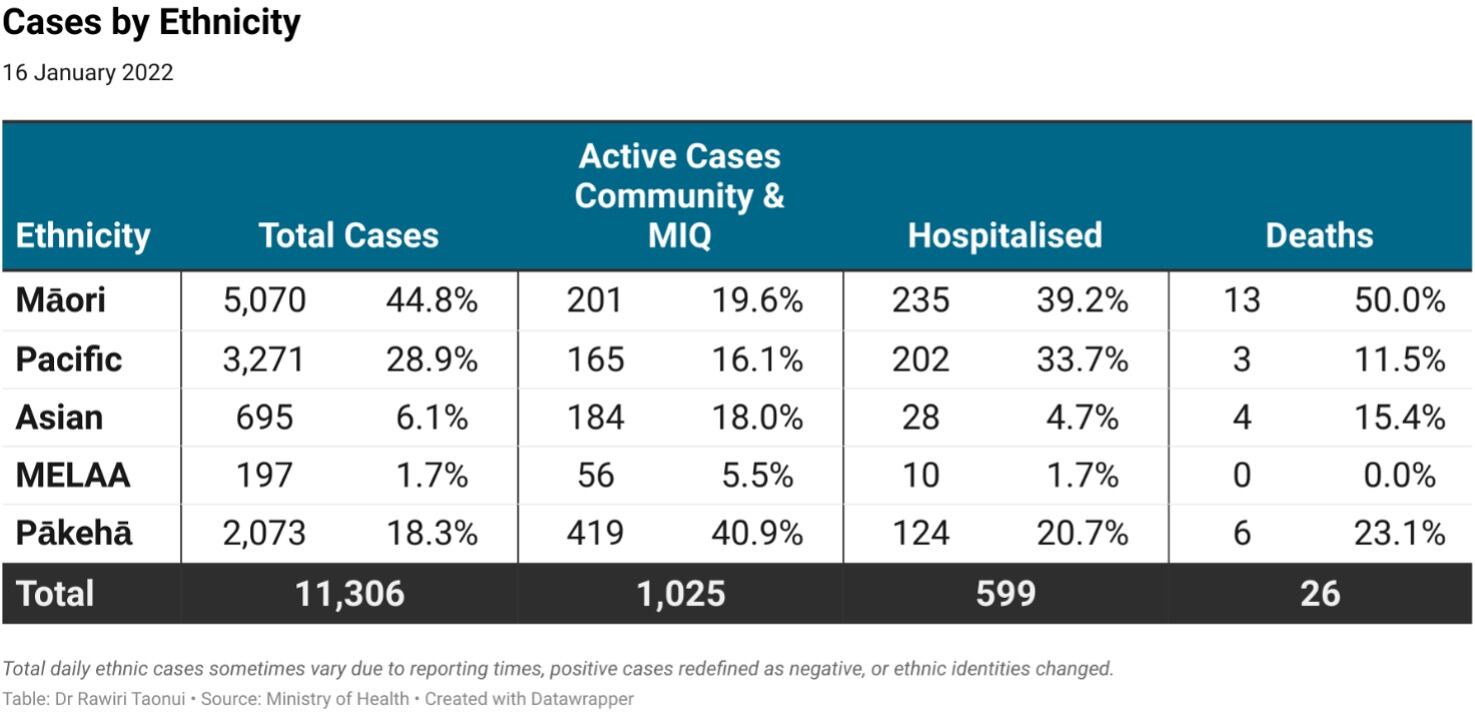
The disturbing tamariki figures reflect the higher disease burden on Māori during the current community outbreak. While Māori make up 17.1 per cent of the population, we make up 44.8 per cent of cases, 39.2 per cent of hospitalisations and 50 per cent of deaths.
The only bright spot, a surge in Pākehā holiday cases seeking fun under a pandemic sun and overseas returnees, means we are no longer the highest number of active cases.
Vaccination discrimination
The disproportionate Māori figures are the direct result of last year’s discriminatory age-based older first younger later vaccine rollout. This approach prevented Māori whānau vaccination, this most effective indigenous immunisation approach used with success in the United States and British Columbia.
The vaccine rollout also privileged 600,000 Pākehā aged 65yrs-plus over more than 100,000 Māori aged 50-64yrs with the same Covid-19 risk profile and pushed Maoridom’s youthful population to the back of the line while creating a void of mistrust that racists, serial tithers and impertinent anti-vaxxers filled with misinformation.
Undercount
Projecting the challenges ahead on one side there will be resistance from anti-vaxxers and on the other the problem of an undercount.
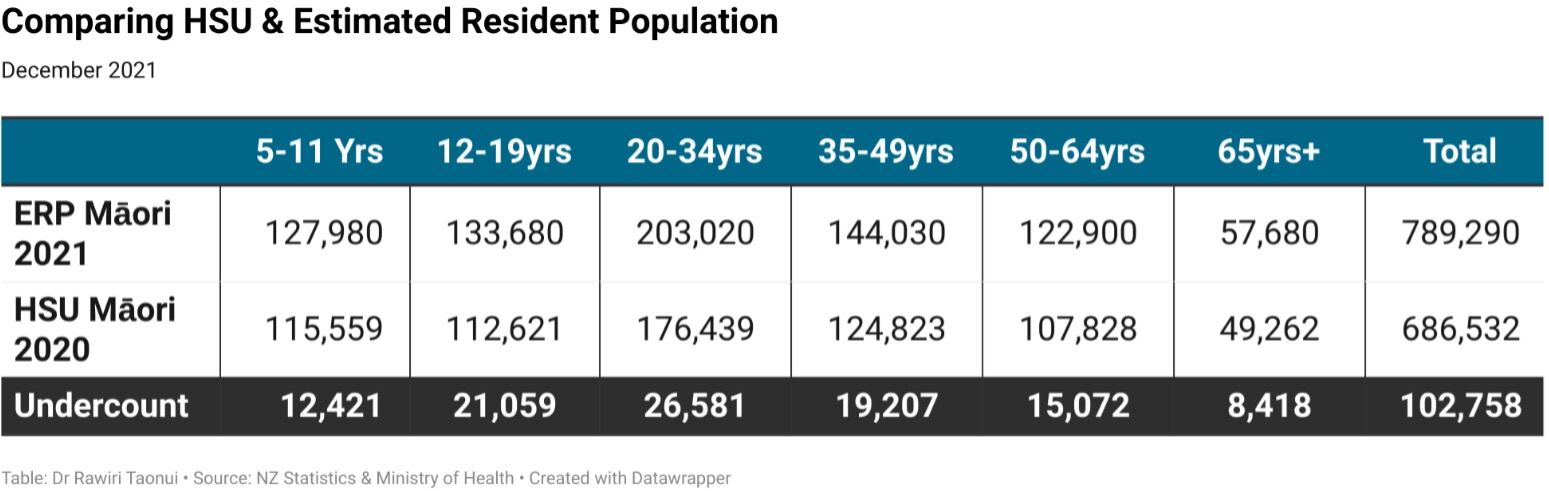
The Ministry of Health utilises the Health Services User index (HSU) to calculate vaccination figures. The HSU is based on the number of people who used the health system in 2020. It does not include those who did not use health services in 2020 because they were extremely healthy, did not trust health services or were too poor. This creates an undercount.
When comparing the HSU with the 2021 NZ Statistics Estimate of the Resident Population (ERP), there is a maximum potential undercount of 102,700 in the vaccine eligible Māori population including 12,420 in the five-to-11-year-olds age group. This figure presents a potential risk whereby a misleading overoptimistic count of progress undermines the vaccination of our youngest and most vulnerable.
Equity vs equality of outcomes
To their credit, the government and ministry are attempting to do better by consulting with Te Rōpū Whakakaupapa Urutā, the main Māori medical experts group, the Iwi Leaders Forum Pandemic Response Group, and other Māori advisers.
For this to be successful it must move beyond equity approaches that emphasise a tick box cultural approach with a capital Kia Ora, consultation without comprehension, and karakia at the beginning and end of hui and zui.
Instead, the tamariki rollout needs to emphasise equal outcomes with Pākehā based on co-management via a Māori vaccination leadership group with oversight on the rollout and strong resourcing for Māori health providers whether iwi-based or centred on the Whānau Ora Commissioning Agency.
Communications must be by Māori for Māori, mirroring the successful IraDot Youngatira campaigns targeting 12-34-year-old Māori. District health Bboards need to learn that Te Tiriti o Waitangi means less talking and more listening and less power over Māori and more empowerment of Māori communities,
On the ground, the tamariki rollout should include vaccination centres working in partnership with Māori authorities. Opportunities must exist for whānau-centred approaches such as combining adult boosters with child shots. And, because the majority of tamariki Māori are clustered in low-decile schools, a focused roll-out there.
Pacific children
The 5-11yrs vaccination rollout priority must also extend to the Pacific community. Pacific peoples are eight per cent of the population but Pacific children make up 28.7 per cent of all under 12yrs cases and 15.2 per cent of hospitalisations.
Pacific and Māori peoples face similar prejudice. Together, our children comprise 82.0 per cent of all under-12yrs cases and 78.3 per cent of all hospitalisations.
This is our brown pandemic. Māori and Pacific are 73.8 per cent of all cases in the outbreak, 73.0 per cent of hospitalisations and 61.5 per cent of deaths.
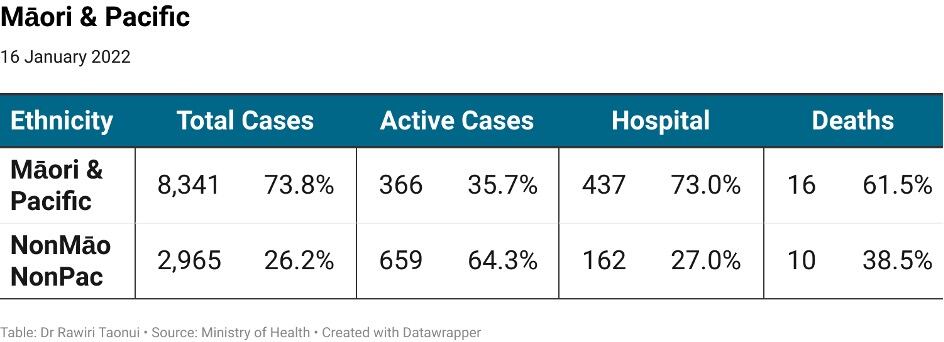
Māori and Pacific have been the highest number of cases 141 times during the 153-day outbreak. Over 70% of the more than 5,000 Auckland cases in four months have been Māori or Pacific.
Māori and Pacific are a considerable number of 892 active cases isolating at home with incumbent risks and two deaths while their rooms in Managed Isolation and Quarantine (MIQ) are freed allowing mainly Pākehā New Zealanders to return home.
Omicron
Data emerging from overseas backs the need to prioritise Māori and Pacific children. Last week, the American Academy of Paediatrics reported a 50 per cent rise to 199,000 child infections and a 66 per cent rise to a record 400 child hospitalisations in one week at the end of December. The lesson, a small percentage of severe young cases amongst an enormous number of mild Omicron cases equals a serious number of cases among the young and vulnerable.
With over 266 Omicron cases in Aotearoa and three Omicron breaches of the border and MIQ, a poor Māori and Pacific child vaccination rollout would cast the darkest of shadows on the already blemished Covid-19 ethnic record of the government and Ministry of Health.
Noho haumaru, stay safe.
Dr Rawiri Taonui has contributed to a Ministry of Health Māori U12yrs Vaccination Working Group.